Bulletin: March 2020 Situation Report – Coronavirus Disease 2019 (COVID-19)
This SITREP is a Public Service Announcement sponsored by The Conceptium Group.
The outbreak of COVID-19 is a rapidly evolving public health crisis that may be termed a global pandemic. SPEAR will provide new information as it becomes available, in addition to updated guidance.
Facts you should know

Electron microscope image shows SARS-CoV-2 (yellow)—aka 2019-nCoV, the virus that causes COVID-19—isolated from a patient in the U.S., emerging from the surface of cells (blue/pink) cultured in the lab.
Background: Common human coronaviruses usually cause mild to moderate upper-respiratory tract illnesses, like the common cold. Most people get infected with one or more of these viruses at some point in their lives. This information applies to common human coronaviruses and should not be confused with COVID-19.
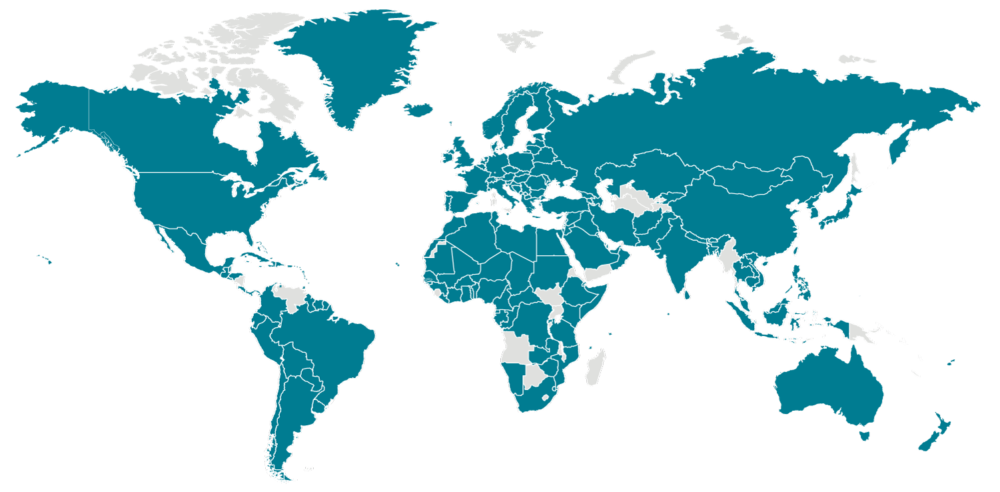
Health authorities worldwide are responding to an outbreak of respiratory disease caused by a novel coronavirus that was first detected in Wuhan Province, China, and which has now been detected in almost 70 locations internationally. The virus has been named “SARS-CoV-2”, and the disease it causes has been named “Coronavirus Disease 2019” (abbreviated “COVID-19”). On January 30th, 2020, the Emergency Committee of the World Health Organization (WHO) declared the outbreak a “Public Health Emergency of International Concern” (PHEIC), which is “an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response”.
Epidemiology – Source and Initial Spread of the Virus
Coronaviruses cause zoonotic disease, transmitting from animals to humans. Coronaviruses are a large family of viruses that are common in people and many different species of animals, including camels, cattle, cats, and bats. Animal coronaviruses can infect people and then spread between people such as with MERS-CoV (Middle East Respiratory Syndrome – Coronavirus), SARS-CoV (Severe Acute Respiratory Syndrome – Coronavirus) – and now SARS-CoV-2. The SARS-CoV-2 virus is a betacoronavirus, like MERS-CoV and SARS-CoV. All three of these viruses have their origins in bats.



Greetings Spear Mission, the challenge still remains that many questions are being asked about the origin of this pandemic, sighting possible espionage or even bio-warfare between leading nations, a dispute gone wrong that is consuming the world as we know it.
Most worrisome is the uncouth way the first alarms raised in China were quelled and the lackadaisical way it was handled in America till it escalated to this nightmare. Whether it was incubated in lab and weaponized, or it surrogates in an animal poached, the fact still remains that our global village is now turning into a graveyard.
If developed countries are struggling to get genuine detection (test) kits, medical ventilators and appropriate medication, what will happen to lesser countries or countries that are not prepared or cannot get any essential commodities to contain their cases? Why is the developed world so selfish and irrational to a point the world over is burying should in hundreds and thousands. If ignorance of the “Black Plague” or lack of knowledge was the issue, at least we would have a fallback position but this is very reckless and appalling.
May the GOD that any of us serve have mercy on our souls if we survive this uninvited killer.
Remain blessed.